What causes acne? Is acne more than skin deep?
Acne, or more accurately acne vulgaris, is one of the most common skin conditions, characterised by clogged pilosebaceous follicles when comedones (small, flesh-coloured raised areas of skin tissue) are formed as a result of increased sebum production and blocked follicular openings, mainly on the face but also on the chest and back. But although the manifestation of acne is visibly on the skin, the cause of acne can sometimes be a symptom of other conditions. Certainly, acne is more than skin deep!
Closed comedones (whiteheads) are formed when there is a complete blockage and open comedones (blackheads) are formed when there is a partial blockage. These may manifest as non-inflammatory lesions, superficial inflammatory lesions (papules, pustules) or deeper inflammatory lesions (nodules, cysts).1 Severe acne, which carries a risk of scarring, is normally referred to a dermatologist for treatment.
Not just a teenage nightmare
Once considered a condition of the teenage population, acne is becoming increasingly prevalent in the adult population.
An incidence is reported of 95% of people aged between 11 and 30 suffering from acne to some extent.2 In addition to the persistent cases of adult acne which are a relapse of adolescent acne, late-onset acne, occurring for the first time, is also recognised.
The incidence of acne is increasing in the population over 25 years.3,4 More commonly affecting males than females aged 16 to 19, in teenagers aged 14 to 17 and adults, the trend is reversed with more females than males affected.4
Acne is often a feature of Polycystic Ovary Syndrome (PCOS). For a diagnosis, women with PCOS have at least two of three symptoms: polycystic ovaries, ovulatory dysfunction, and androgen excess.5 The presence of acne has been attributed to the high androgens of the condition. Acne associated with PCOS, however, needs to be viewed within the whole context of PCOS and in relation to other common features of the syndrome, in particular obesity and insulin resistance.
If you are an adult suffering from acne, in addition to the physical pain of the condition, you may be aware that you are more vulnerable to the distressing experiences of low self-esteem, negative body image, anxiety and depression.4,6
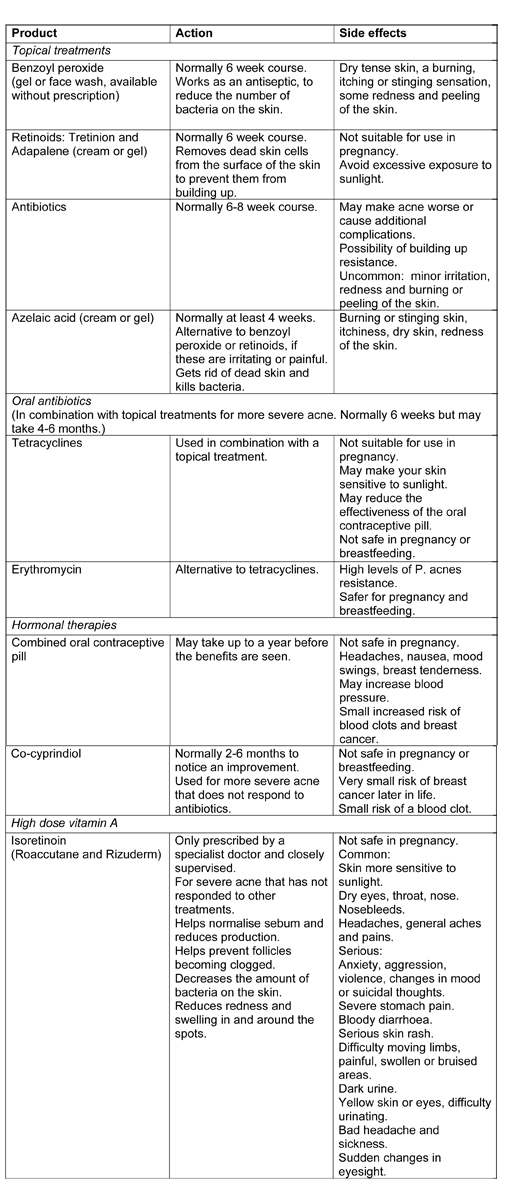
Convention treatments for acne
Although a common response to an outbreak of acne is to use makeup to cover up, this may provide a quick fix but in fact may also clog pores and worsen acne, as may some skincare products. In addition to non-pharmaceutical treatments, including a comedone extractor, chemical peels and photodynamic therapy, there is a range of pharmaceutical treatments used for acne, including over-the-counter products and medication on prescription. A combination of antibiotic tablets and topical treatments is often the first treatment option.2
Is skin clear of acne just a dream?
Many of the conventional treatments for acne take 2 to 3 months before they start to work, with the potential for undesirable and even very serious side effects, and no guarantee that the acne will not come back. A limitation of the medications for acne is that they are designed only to treat the symptoms and not to address the root causes of acne. However, acne is a multifactorial, inflammatory condition.4,9
Acne is only cleared completely when the root causes are addressed.
Genes may influence the development of acne, but there are other factors, including hormonal, inflammatory and environmental influences. Androgens (male sex hormones) have often been considered the cause of acne, but other hormones (such as insulin), are implicated in the complexity of its pathogenesis.3
Other factors implicated in the development of acne include the immune system and stess.4 Equilibiurm of the skin microbiome has a role in acne. While Probionibacterium acnes (renamed Cutibacterium acnes) supports a healthy skin, it may also become an opportunistic pathogen.7
Skin clear of acne does not have to be a dream. Acknowledging that acne is more than skin deep, and therefore topical treatments are not the best solution, is a good starting point. There is an alternative to the limitations of treating only the symptoms, with the prospect of side effects and unpredictable outcomes. Clearing acne by addressing its pathogenesis, with a functional medicine approach, is based on:
- Identifying and addressing the root causes of acne in the systems of the body
- Recognising that everyone is unique and that each person’s root causes are individual
Can food cause or clear acne?
The evidence of a number of global studies of indigenous societies points to a relationship between food and acne, particularly in the development of acne in these societies when they have adopted a Western diet.
At the time when they were following their traditional diets, studies found that there was no acne in the populations of the Canadian Inuit, South African Zulus, Japanese Okinawans, Aché of Paraguay and Kitavan islanders of Papua New Guinea.8 A change has only occurred when these societies have adopted a Western diet, and the prevalence of acne has emerged to a level similar to other Western societies.
Two of the foods with a reputation for causing acne are chocolate and milk (dairy). Will giving up milk and chocolate clear your acne?
Although chocolate has been widely accepted as causing acne, studies have not been conclusive.1,9 In studies that have found a link, it is not clear whether it is the cocoa itself or the other ingredients (sugar and fats) of chocolate bars that are implicated.1
Some studies have found that seems to be a link between dairy consumption and acne. Milk has too many components to have a basic chemical formula; it is a very complex mixture of water, fats, proteins and carbohydrates. It is not clear which components of the milk (such as hormones, whey or fat) may be implicated in the development of acne.1,8
The relationship between the Glycaemic Index (GI) of foods and acne has been widely studied. The GI of a food is a measure of the rise in the level of blood glucose, relative to pure glucose, after the food has been consumed. Studies have found an association between high GI levels and acne. Evidence has been found that a low GI diet seems to be associated with an improvement in acne symptoms.9
While further studies may provide more conclusive results about the relationship between specific foods and acne for individuals, decisions about giving up a food need to balance the benefits of giving up the food with the restrictive impact, such as the potential loss of nutrients and impact on other aspects of health. However, a low GI diet, likely to have a positive impact on improving acne, is likely to have other benefits for health, such as weight loss and lowering blood sugar levels, with benefits for cardiovascular health and decreased risk of diabetes type 2. There are many commonalities between a Mediterranean Diet and a low GI diet.
As everyone’s physiology and bio-chemistry is individual, the drivers of acne vary between individuals. With differences in the drivers of acne, some people may benefit by implementing only a simple change, whereas others may need to implement a few changes, to clear acne.
The most effective therapeutic plan is personalised for the specific drivers of each individual. When the drivers of acne present a more complex picture, the results of functional medicine testing are helpful to inform a detailed assessment of the specific drivers of acne. A naturopathic nutritional approach, based on scientific evidence, prioritises a personalised assessment to identify the specific nutrients and lifestyle for the individual to clear acne.
A whole-body perspective
As the largest organ in your body, your skin is an integral part of your body. Acne is a symptom reflecting the health and wellbeing of other systems within: the outward manifestations of acne represent something that is far more than skin deep.
The effective way to clear acne is both from the outside, with the right skincare routines, and from the inside, by addressing the root causes of acne at a cellular level through diet and lifestyle. The misery of acne does not have to be part of your life.

Jane Hickey is a registered nutritional therapist, creating individualised plans for clients to support their health and wellbeing.
Website: janehickeynutrition.com
Telephone: 07305 531583
Email: jane@janehickeynutrition.com
References:
- E H Spencer Diet and acne: a review of the evidence (2009)
- nhs.uk/conditions/acne/treatment (2019)
- V Goulden, S M Clark & W J Cunliffe Post-adolescent acne: a review of clinical features (2008)
- Skroza MD Adult Acne Versus Adolescent Acne: A Retrospective study of 1,167 patients (2018)
- W Duncan A guide to understanding polycystic ovary syndrome (2014)
- Anna Hwee Sing Heng Systematic review of the epidemiology of acne vulgaris (2020)
- B Dréno, S Pécastaings, S Corvec, S Veraldi, A Khammari & C Roques Cutibacterium acnes (Propiobacterium acnes) and acne vulgaris: a brief look at the latest updates (2018)
- L Cordain, S Lindeberg, M Hurtadao, K Hill, S Boyd Eaton & J Brand-Miller Acne Vulgaris A Disease of Western Civilization (2002)
- Hilary Baldwin & Jerry Tan Effects of Diet on Acne and Its Response to Treatment (2020)


2 Comments
[…] Naturally, the first cause of action is to do as much as possible to prevent acne in the first place. […]
[…] As nutritionist Jane Hickey emphasises in her article Acne is more than skin deep: […]